A mediation analysis of the influence of sleep on the relationship between smartphone screen time and youth mental health
Vol.19,No.5(2025)
Research using subjective measures suggests that young people spend large amounts of their leisure time using digital media, which may affect their mental health. Of particular concern is that smartphone screen-time may replace health-promoting activities such as sleep and thereby contribute to mental health problems. Considering that previous studies primarily relied on subjective reports of screen-time and its effects on youth mental health, the objective of the current research was to examine whether screen-time objectively measured via mobile sensing was associated with internalizing (e.g., anxiety, depression) and externalizing (e.g., impulsivity, aggression) symptoms and whether this association was mediated by reduced sleep duration. 407 Canadian youths aged 15–25 completed questionnaires about their mental health symptoms and used a mobile sensing app to measure screen-time and sleep for at least 14 days. The association between screen-time and mental health symptoms and the mediation of sleep duration were tested by fitting structural equation models. Results suggested that objectively measured smartphone screen-time was indirectly associated with externalizing symptoms through reduced sleep duration, but showed no significant association with internalizing symptoms. These findings complement previous research that used subjective measures and highlight the need to provide support and resources to youth to promote healthy screen use and healthy sleep habits.
screen-time; youth mental health; mobile sensing
Silvia Marin-Dragu
Department of Psychiatry, Dalhousie University, Halifax, NS
Silvia Marin-Dragu is currently a graduate student in the Clinical Psychology PhD program at Dalhousie University (Nova Scotia, Canada), and her research work focuses on the intersectionality between technology and youth mental health, under the supervision of Dr. Sandra Meier.
Matt Orr
Department of Psychiatry, Dalhousie University, Halifax, NS
Dr. Matt Orr is a postdoctoral researcher examining novel technologies used to modify or measure the behaviour of children and youth. Dr. Orr also holds a position as Assistant Professor at Acadia University in Nova Scotia, Canada.
Penny Corkum
Department of Psychology and Neuroscience, Dalhousie University, Halifax, NS
Dr. Penny Corkum is a Professor in the Department of Psychology and Neuroscience at Dalhousie University. She has conducted extensive clinical research in the areas of child psychopathology and pediatric sleep, with a particular interest on eHealth.
Benjamin Rusak
Department of Psychiatry, Dalhousie University, Halifax, NS
Dr. Benjamin Rusak is Professor Emeritus in the Department of Psychiatry at Dalhousie University. His extensive research work has focused on investigating mechanism regulating circadian rhythms and sleep, and how they affect cognition, mood, and the risk of developing psychiatric disorders.
Alexa Bagnell
Department of Psychiatry, Dalhousie University, Halifax, NS
Dr. Alexa Bagnell is the Chief of Psychiatry at the IWK Health Centre, as well as Professor in the Department of Psychiatry at Dalhousie University. Dr. Bagnell’s extensive clinical and research work focus on promoting earlier intervention for mental health disorders, with the goal of improving health outcomes in youth.
Sandra Meier
Department of Psychiatry, Dalhousie University, Halifax, NS
Dr. Sandra Meier is an Associate Professor in the Department of Psychiatry at Dalhousie University. Her research focuses on leveraging modern technology to improve mental health care in youth. With her team she has developed an extensive number of apps and smartphone-delivered interventions that have contributed to successfully improving mental health outcomes.
Abi-Jaoude, E., Naylor, K. T., & Pignatiello, A. (2020). Smartphones, social media use and youth mental health. CMAJ, 192(6), E136–E141. https://doi.org/10.1503/cmaj.190434
Alonzo, R., Hussain, J., Stranges, S., & Anderson, K. K. (2021). Interplay between social media use, sleep quality, and mental health in youth: A systematic review. Sleep Medicine Reviews, 56, Article 101414. https://doi.org/10.1016/j.smrv.2020.101414
Ancoli-Israel, S., Cole, R., Alessi, C., Chambers, M., Moorcroft, W., & Pollak, C. P. (2003). The role of actigraphy in the study of sleep and circadian rhythms. Sleep, 26(3), 342–392. https://doi.org/10.1093/sleep/26.3.342
Arundell, L., Salmon, J., Veitch, J., & Timperio, A. (2019). The relationship between objectively measured and self-reported sedentary behaviours and social connectedness among adolescents. International Journal of Environmental Research and Public Health, 16(2), Article 277. https://doi.org/10.3390/ijerph16020277
Atherton, O. E., Ferrer, E., & Robins, R. W. (2018). The development of externalizing symptoms from late childhood through adolescence: A longitudinal study of Mexican-origin youth. Developmental Psychology, 54(6), 1135–1147. https://doi.org/10.1037/dev0000489
Benenson, Z., Gassmann, F., & Reinfelder, L. (2013). Android and iOS users’ differences concerning security and privacy. CHI ’13 Extended Abstracts on Human Factors in Computing Systems, 817–822. https://doi.org/10.1145/2468356.2468502
Boase, J., & Ling, R. (2013). Measuring mobile phone use: Self‐report versus log data. Journal of Computer-Mediated Communication, 18(4), 508–519. https://doi.org/10.1111/jcc4.12021
Boers, E., Afzali, M. H., Newton, N., & Conrod, P. (2019). Association of screen time and depression in adolescence. JAMA Pediatrics, 173(9), 853–859. https://doi.org/10.1001/jamapediatrics.2019.1759
Borger, J. N., Huber, R., & Ghosh, A. (2019). Capturing sleep-wake cycles by using day-to-day smartphone touchscreen interactions. NPJ Digital Medicine, 2, Article 73. https://doi.org/10.1038/s41746-019-0147-4
Buysse, D. J. (2014). Sleep health: Can we define it? Does it matter? Sleep, 37(1), 9–17. https://doi.org/10.5665/sleep.3298
Cain, N., & Gradisar, M. (2010). Electronic media use and sleep in school-aged children and adolescents: A review. Sleep Medicine, 11(8), 735–742. https://doi.org/10.1016/j.sleep.2010.02.006
Cao, H., Qian, Q., Weng, T., Yuan, C., Sun, Y., Wang, H., & Tao, F. (2011). Screen time, physical activity and mental health among urban adolescents in China. Preventive Medicine, 53(4–5), 316–320. https://doi.org/10.1016/j.ypmed.2011.09.002
Cao, J., Truong, A. L., Banu, S., Shah, A. A., Sabharwal, A., & Moukaddam, N. (2020). Tracking and predicting depressive symptoms of adolescents using smartphone-based self-reports, parental evaluations, and passive phone sensor data: Development and usability study. JMIR Mental Health, 7(1), Article e14045. https://doi.org/10.2196/14045
Cavalli, E., Anders, R., Chaussoy, L., Herbillon, V., Franco, P., & Putois, B. (2021). Screen exposure exacerbates ADHD symptoms indirectly through increased sleep disturbance. Sleep Medicine, 83, 241–247. https://doi.org/10.1016/j.sleep.2021.03.010
Chang, A.-M., Aeschbach, D., Duffy, J. F., & Czeisler, C. A. (2015). Evening use of light-emitting eReaders negatively affects sleep, circadian timing, and next-morning alertness. Proceedings of the National Academy of Sciences, 112(4), 1232–1237. https://doi.org/10.1073/pnas.1418490112
Chen, F. F. (2007). Sensitivity of goodness of fit indexes to lack of measurement invariance. Structural Equation Modeling: A Multidisciplinary Journal, 14(3), 464–504. https://doi.org/10.1080/10705510701301834
Cheung, G. W., & Rensvold, R. B. (2002). Evaluating goodness-of-fit indexes for testing measurement invariance. Structural Equation Modeling: A Multidisciplinary Journal, 9(2), 233–255. https://doi.org/10.1207/S15328007SEM0902_5
Ciman, M., & Wac, K. (2019). Smartphones as sleep duration sensors: Validation of the iSenseSleep algorithm. JMIR mHealth and uHealth, 7(5), Article e11930. https://doi.org/10.2196/11930
Combertaldi, S. L., Ort, A., Cordi, M., Fahr, A., & Rasch, B. (2021). Pre-sleep social media use does not strongly disturb sleep: A sleep laboratory study in healthy young participants. Sleep Medicine, 87, 191–202. https://doi.org/10.1016/j.sleep.2021.09.009
Da Costa, B. G. G., Chaput, J.-P., Lopes, M. V. V., Malheiros, L. E. A., Da Silva, I. C. M., & Silva, K. S. (2021). Association between screen time and accelerometer-measured 24-h movement behaviors in a sample of Brazilian adolescents. Public Health, 195, 32–38. https://doi.org/10.1016/j.puhe.2021.03.029
Deyo, A., Wallace ,Josh, & and Kidwell, K. M. (2024). Screen time and mental health in college students: Time in nature as a protective factor. Journal of American College Health, 72(8), 3025–3032. https://doi.org/10.1080/07448481.2022.2151843
Dissing, A. S., Andersen, T. O., Jensen, A. K., Lund, R., & Rod, N. H. (2022). Nighttime smartphone use and changes in mental health and wellbeing among young adults: A longitudinal study based on high-resolution tracking data. Scientific Reports, 12(1), Article 1. https://doi.org/10.1038/s41598-022-10116-z
Druijff-van de Woestijne, G. B., McConchie, H., de Kort, Y. A. W., Licitra, G., Zhang, C., Overeem, S., & Smolders, K. C. H. J. (2021). Behavioural biometrics: Using smartphone keyboard activity as a proxy for rest–activity patterns. Journal of Sleep Research, 30(5), Article e13285. https://doi.org/10.1111/jsr.13285
Eirich, R., McArthur, B. A., Anhorn, C., McGuinness, C., Christakis, D. A., & Madigan, S. (2022). Association of screen time with internalizing and externalizing behavior problems in children 12 years or younger: A systematic review and meta-analysis. JAMA Psychiatry, 79(5), 393–405. https://doi.org/10.1001/jamapsychiatry.2022.0155
Elhai, J. D., Levine, J. C., & Hall, B. J. (2019). The relationship between anxiety symptom severity and problematic smartphone use: A review of the literature and conceptual frameworks. Journal of Anxiety Disorders, 62, 45–52. https://doi.org/10.1016/j.janxdis.2018.11.005
Elhai, J. D., Yang, H., Fang, J., Bai, X., & Hall, B. J. (2020). Depression and anxiety symptoms are related to problematic smartphone use severity in Chinese young adults: Fear of missing out as a mediator. Addictive Behaviors, 101, Article 105962. https://doi.org/10.1016/j.addbeh.2019.04.020
Ellis, D. A., Davidson, B. I., Shaw, H., & Geyer, K. (2019). Do smartphone usage scales predict behavior? International Journal of Human-Computer Studies, 130, 86–92. https://doi.org/10.1016/j.ijhcs.2019.05.004
Exelmans, L., & Van den Bulck, J. (2019). Sleep research: A primer for media scholars. Health Communication, 34(5), 519–528. https://doi.org/10.1080/10410236.2017.1422100
Fassi, L., Ferguson, A. M., Przybylski, A. K., Ford, T. J., & Orben, A. (2025). Social media use in adolescents with and without mental health conditions. Nature Human Behaviour, 9(6), 1283–1299. https://doi.org/10.1038/s41562-025-02134-4
Ferguson, C. J. (2011). The influence of television and video game use on attention and school problems: A multivariate analysis with other risk factors controlled. Journal of Psychiatric Research, 45(6), 808–813. https://doi.org/10.1016/j.jpsychires.2010.11.010
Galea, S., & Tracy, M. (2007). Participation rates in epidemiologic studies. Annals of Epidemiology, 17(9), 643–653. https://doi.org/10.1016/j.annepidem.2007.03.013
Garcia, K. K. S., & Abrahão, A. A. (2021). Research development using REDCap software. Healthcare Informatics Research, 27(4), 341–349. https://doi.org/10.4258/hir.2021.27.4.341
Giorgi, F. M., Ceraolo, C., & Mercatelli, D. (2022). The R language: An engine for bioinformatics and data science. Life, 12(5), Article 648. https://doi.org/10.3390/life12050648
Godsell, S., & White, J. (2019). Adolescent perceptions of sleep and influences on sleep behaviour: A qualitative study. Journal of Adolescence, 73(1), 18–25. https://doi.org/10.1016/j.adolescence.2019.03.010
Goodman, R. (1997). The strengths and difficulties questionnaire: A research note. Journal of Child Psychology and Psychiatry, 38(5), 581–586. https://doi.org/10.1111/j.1469-7610.1997.tb01545.x
Goodman, R. (2001). Psychometric properties of the strengths and difficulties questionnaire. Journal of the American Academy of Child & Adolescent Psychiatry, 40(11), 1337–1345. https://doi.org/10.1097/00004583-200111000-00015
Goodman, R., & Scott, S. (1999). Comparing the strengths and difficulties questionnaire and the child behavior checklist: Is small beautiful? Journal of Abnormal Child Psychology, 27(1), 17–24. https://doi.org/10.1023/A:1022658222914
Government of Canada, S. C. (2021a, June 21). Smartphone use and smartphone habits by gender and age group, inactive. https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=2210011501
Government of Canada, S. C. (2021b, November 17). Guide to the census of population. https://www12.statcan.gc.ca/census-recensement/2021/ref/98-304/index-eng.cfm
Guerrero, M. D., Barnes, J. D., Chaput, J.-P., & Tremblay, M. S. (2019). Screen time and problem behaviors in children: Exploring the mediating role of sleep duration. International Journal of Behavioral Nutrition and Physical Activity, 16(1), Article 105. https://doi.org/10.1186/s12966-019-0862-x
Hale, L., & Guan, S. (2015). Screen time and sleep among school-aged children and adolescents: A systematic literature review. Sleep Medicine Reviews, 21, 50–58. https://doi.org/10.1016/j.smrv.2014.07.007
Heo, J.-Y., Kim, K., Fava, M., Mischoulon, D., Papakostas, G. I., Kim, M.-J., Kim, D. J., Chang, K.-A. J., Oh, Y., Yu, B.-H., & Jeon, H. J. (2017). Effects of smartphone use with and without blue light at night in healthy adults: A randomized, double-blind, cross-over, placebo-controlled comparison. Journal of Psychiatric Research, 87, 61–70. https://doi.org/10.1016/j.jpsychires.2016.12.010
Hoge, E., Bickham, D., & Cantor, J. (2017). Digital media, anxiety, and depression in children. Pediatrics, 140(Supplement 2), S76–S80. https://doi.org/10.1542/peds.2016-1758G
Hosokawa, R., & Katsura, T. (2017). A longitudinal study of socioeconomic status, family processes, and child adjustment from preschool until early elementary school: The role of social competence. Child and Adolescent Psychiatry and Mental Health, 11(1), Article 62. https://doi.org/10.1186/s13034-017-0206-z
Jackson, M. I., Kiernan, K., & McLanahan, S. (2017). Maternal education, changing family circumstances, and children’s skill development in the United States and UK. The Annals of the American Academy of Political and Social Science, 674(1), 59–84. https://doi.org/10.1177/0002716217729471
Johnson, J. G., Cohen, P., Kasen, S., & Brook, J. S. (2007). Extensive television viewing and the development of attention and learning difficulties during adolescence. Archives of Pediatrics & Adolescent Medicine, 161(5), 480–486. https://doi.org/10.1001/archpedi.161.5.480
Joshi, S. C. (2022). Sleep latency and sleep disturbances mediates the association between nighttime cell phone use and psychological well-being in college students. Sleep and Biological Rhythms, 20(3), 431–443. https://doi.org/10.1007/s41105-022-00388-3
Landoll, R. R., La Greca, A. M., Lai, B. S., Chan, S. F., & Herge, W. M. (2015). Cyber victimization by peers: Prospective associations with adolescent social anxiety and depressive symptoms. Journal of Adolescence, 42(1), 77–86. https://doi.org/10.1016/j.adolescence.2015.04.002
Leung, C. Y., & Torres, R. (2021). Sleep duration does not mediate the association between screen time and adolescent depression and anxiety: Findings from the 2018 National Survey of Children’s Health. Sleep Medicine, 81, 227–234. https://doi.org/10.1016/j.sleep.2021.02.031
Li, X., Buxton, O. M., Lee, S., Chang, A.-M., Berger, L. M., & Hale, L. (2019). Sleep mediates the association between adolescent screen time and depressive symptoms. Sleep Medicine, 57, 51–60. https://doi.org/10.1016/j.sleep.2019.01.029
Li, X., Vanderloo, L. M., Keown-Stoneman, C. D. G., Cost, K. T., Charach, A., Maguire, J. L., Monga, S., Crosbie, J., Burton, C., Anagnostou, E., Georgiades, S., Nicolson, R., Kelley, E., Ayub, M., Korczak, D. J., & Birken, C. S. (2021). Screen use and mental health symptoms in Canadian children and youth during the COVID-19 pandemic. JAMA Network Open, 4(12), Article e2140875. https://doi.org/10.1001/jamanetworkopen.2021.40875
Liu, Y., Sun, Y., Zheng, K., Zheng, J., Kong, L., Gu, J., & Huang, T. (2023). Association of screen time with anxiety and depressive symptoms in college students during COVID-19 outbreak in Shanghai: Mediation role of sleep quality. Cyberpsychology, Behavior, and Social Networking, 26(10), 755-763. https://doi.org/10.1089/cyber.2022.0373
MacLeod, L., Suruliraj, B., Gall, D., Bessenyei, K., Hamm, S., Romkey, I., Bagnell, A., Mattheisen, M., Muthukumaraswamy, V., Orji, R., & Meier, S. (2021). A mobile sensing app to monitor youth mental health: Observational pilot study. JMIR mHealth and uHealth, 9(10), Article e20638. https://doi.org/10.2196/20638
Madigan, S., Browne, D., Racine, N., Mori, C., & Tough, S. (2019). Association between screen time and children’s performance on a developmental screening test. JAMA Pediatrics, 173(3), 244–250. https://doi.org/10.1001/jamapediatrics.2018.5056
Madigan, S., Eirich, R., Pador, P., McArthur, B. A., & Neville, R. D. (2022). Assessment of changes in child and adolescent screen time during the COVID-19 pandemic: A systematic review and meta-analysis. JAMA Pediatrics, 176(12), 1188–1198. https://doi.org/10.1001/jamapediatrics.2022.4116
Mathers, M., Canterford, L., Olds, T., Hesketh, K., Ridley, K., & Wake, M. (2009). Electronic media use and adolescent health and well-being: Cross-sectional community study. Academic Pediatrics, 9(5), 307–314. https://doi.org/10.1016/j.acap.2009.04.003
Maxwell, S. E., Cole, D. A., & Mitchell, M. A. (2011). Bias in cross-sectional analyses of longitudinal mediation: Partial and complete mediation under an autoregressive model. Multivariate Behavioral Research, 46(5), 816–841. https://doi.org/10.1080/00273171.2011.606716
McDaniel, B. T., & Radesky, J. S. (2020). Longitudinal associations between early childhood externalizing behavior, parenting stress, and child media use. Cyberpsychology, Behavior, and Social Networking, 23(6), 384–391. https://doi.org/10.1089/cyber.2019.0478
Meyerhoff, J., Liu, T., Kording, K. P., Ungar, L. H., Kaiser, S. M., Karr, C. J., & Mohr, D. C. (2021). Evaluation of changes in depression, anxiety, and social anxiety using smartphone sensor features: Longitudinal cohort study. Journal of Medical Internet Research, 23(9), Article e22844. https://doi.org/10.2196/22844
Nagata, J. M., Cortez, C. A., Cattle, C. J., Ganson, K. T., Iyer, P., Bibbins-Domingo, K., & Baker, F. C. (2021). Screen time use among US adolescents during the COVID-19 pandemic: Findings from the adolescent brain cognitive development (ABCD) study. JAMA Pediatrics. https://doi.org/10.1001/jamapediatrics.2021.4334
Neville, R. D., McArthur, B. A., Eirich, R., Lakes, K. D., & Madigan, S. (2021). Bidirectional associations between screen time and children’s externalizing and internalizing behaviors. Journal of Child Psychology and Psychiatry, 62(12), 1475–1484. https://doi.org/10.1111/jcpp.13425
Orben, A., & Przybylski, A. K. (2019). Screens, teens, and psychological well-being: Evidence from three time-use-diary studies. Psychological Science, 30(5), 682–696. https://doi.org/10.1177/0956797619830329
Otte Andersen, T., Skovlund Dissing, A., Rosenbek Severinsen, E., Kryger Jensen, A., Thanh Pham, V., Varga, T. V., & Hulvej Rod, N. (2022). Predicting stress and depressive symptoms using high-resolution smartphone data and sleep behavior in Danish adults. Sleep, 45(6), Article zsac067. https://doi.org/10.1093/sleep/zsac067
Pang, H. (2022). Connecting mobile social media with psychosocial well-being: Understanding relationship between WeChat involvement, network characteristics, online capital and life satisfaction. Social Networks, 68, 256–263. https://doi.org/10.1016/j.socnet.2021.08.006
Parker, H., Burkart, S., Reesor-Oyer, L., Smith, M. T., Dugger, R., von Klinggraeff, L., Weaver, R. G., Beets, M. W., & Armstrong, B. (2022). Feasibility of measuring screen time, activity, and context among families with preschoolers: Intensive longitudinal pilot study. JMIR Formative Research, 6(9), Article e40572. https://doi.org/10.2196/40572
Parry, D. A., Davidson, B. I., Sewall, C. J. R., Fisher, J. T., Mieczkowski, H., & Quintana, D. S. (2021). A systematic review and meta-analysis of discrepancies between logged and self-reported digital media use. Nature Human Behaviour, 5(11), 1535–1547. https://doi.org/10.1038/s41562-021-01117-5
Pedersen, J., Rasmussen, M. G. B., Sørensen, S. O., Mortensen, S. R., Olesen, L. G., Brønd, J. C., Brage, S., Kristensen, P. L., & Grøntved, A. (2022). Effects of limiting recreational screen media use on physical activity and sleep in families with children: A cluster randomized clinical trial. JAMA Pediatrics, 176(8), 741–749. https://doi.org/10.1001/jamapediatrics.2022.1519
Peltonen, E., Lagerspetz, E., Hamberg, J., Mehrotra, A., Musolesi, M., Nurmi, P., & Tarkoma, S. (2018). The hidden image of mobile apps: Geographic, demographic, and cultural factors in mobile usage. In Proceedings of the 20th International Conference on Human-Computer Interaction with Mobile Devices and Services (pp. 1–12). ACM. https://doi.org/10.1145/3229434.3229474
Primack, B. A., Swanier, B., Georgiopoulos, A. M., Land, S. R., & Fine, M. J. (2009). Association between media use in adolescence and depression in young adulthood: A longitudinal study. Archives of General Psychiatry, 66(2), 181–188. https://doi.org/10.1001/archgenpsychiatry.2008.532
Przybylski, A. K., & Weinstein, N. (2017). A large-scale test of the Goldilocks hypothesis: Quantifying the relations between digital-screen use and the mental well-being of adolescents. Psychological Science, 28(2), 204–215. https://doi.org/10.1177/0956797616678438
Ra, C. K., Cho, J., Stone, M. D., De La Cerda, J., Goldenson, N. I., Moroney, E., Tung, I., Lee, S. S., & Leventhal, A. M. (2018). Association of digital media use with subsequent symptoms of attention-deficit/hyperactivity disorder among adolescents. JAMA, 320(3), 255–263. https://doi.org/10.1001/jama.2018.8931
Ribner, A. D., Coulanges, L., Friedman, S., Libertus, M. E., & I-FAM-Covid Consortium. (2021). Screen time in the Coronavirus 2019 era: International trends of increasing use among 3- to 7-year-old children. The Journal of Pediatrics, 239, 59–66.e1. https://doi.org/10.1016/j.jpeds.2021.08.068
Riehm, K. E., Feder, K. A., Tormohlen, K. N., Crum, R. M., Young, A. S., Green, K. M., Pacek, L. R., La Flair, L. N., & Mojtabai, R. (2019). Associations between time spent using social media and internalizing and externalizing problems among US youth. JAMA Psychiatry, 76(12), 1266–1273. https://doi.org/10.1001/jamapsychiatry.2019.2325
Rosseel, Y. (2012). lavaan: An R package for structural equation modeling. Journal of Statistical Software, 48(2),
1–36. https://doi.org/10.18637/jss.v048.i02
Sanders, T., Parker, P. D., Del Pozo-Cruz, B., Noetel, M., & Lonsdale, C. (2019). Type of screen time moderates effects on outcomes in 4013 children: Evidence from the longitudinal study of Australian children. The International Journal of Behavioral Nutrition and Physical Activity, 16(1), Article 117. https://doi.org/10.1186/s12966-019-0881-7
Santos, R. M. S., Ventura, S. de A., Nogueira, Y. J. de A., Mendes, C. G., Paula, J. J. de, Miranda, D. M., & Romano-Silva, M. A. (2024). The associations between screen time and mental health in adults: A systematic review. Journal of Technology in Behavioral Science, 9(4), 825–845. https://doi.org/10.1007/s41347-024-00398-7
Tandon, A., Dhir, A., Almugren, I., AlNemer, G. N., & Mäntymäki, M. (2021). Fear of missing out (FoMO) among social media users: A systematic literature review, synthesis and framework for future research. Internet Research, 31(3), 782–821. https://doi.org/10.1108/INTR-11-2019-0455
Tapia-Serrano, M. A., Sevil-Serrano, J., Sánchez-Miguel, P. A., López-Gil, J. F., Tremblay, M. S., & García-Hermoso, A. (2022). Prevalence of meeting 24-hour movement guidelines from pre-school to adolescence: A systematic review and meta-analysis including 387,437 participants and 23 countries. Journal of Sport and Health Science, 11(4), 427–437. https://doi.org/10.1016/j.jshs.2022.01.005
Tarokh, L., Saletin, J. M., & Carskadon, M. A. (2016). Sleep in adolescence: Physiology, cognition and mental health. Neuroscience & Biobehavioral Reviews, 70, 182–188. https://doi.org/10.1016/j.neubiorev.2016.08.008
Torous, J., Kiang, M. V., Lorme, J., & Onnela, J.-P. (2016). New tools for new research in psychiatry: A scalable and customizable platform to empower data driven smartphone research. JMIR Mental Health, 3(2), Article e16. https://doi.org/10.2196/mental.5165
Touitou, Y., Touitou, D., & Reinberg, A. (2016). Disruption of adolescents’ circadian clock: The vicious circle of media use, exposure to light at night, sleep loss and risk behaviors. Journal of Physiology-Paris, 110(4), 467–479. https://doi.org/10.1016/j.jphysparis.2017.05.001
Twenge, J. M., & Campbell, W. K. (2018). Associations between screen time and lower psychological well-being among children and adolescents: Evidence from a population-based study. Preventive Medicine Reports, 12, 271–283. https://doi.org/10.1016/j.pmedr.2018.10.003
Vahedi, Z., Sibalis, A., & Sutherland, J. E. (2018). Are media literacy interventions effective at changing attitudes and intentions towards risky health behaviors in adolescents? A meta-analytic review. Journal of Adolescence, 67(1), 140–152. https://doi.org/10.1016/j.adolescence.2018.06.007
van de Schoot, R., Lugtig, P., & Hox, J. (2012). A checklist for testing measurement invariance. European Journal of Developmental Psychology, 9(4), 486–492. https://doi.org/10.1080/17405629.2012.686740
Verma, S., Vandana, P., Soda, T., Koth, K. A., Aguayo, P., Shaffer, R. C., Hellings, J., & Muhle, R. A. (2022). Incorporation of telepsychiatry for patients with developmental disorders into routine clinical practice—A survey of specialty clinics adapting to telepsychiatry during the COVID-19 pandemic. Journal of Autism and Developmental Disorders, 52(12), 5280–5284. https://doi.org/10.1007/s10803-022-05593-0
Vernon, L., Modecki, K. L., & Barber, B. L. (2018). Mobile phones in the bedroom: Trajectories of sleep habits and subsequent adolescent psychosocial development. Child Development, 89(1), 66–77. https://doi.org/10.1111/cdev.12836
Viner, R., Gireesh, A., Stiglic, N., Hudson, L., Goddings, A.-L., Ward, J., & Nicholls, D. (2019). Roles of cyberbullying, sleep, and physical activity in mediating the effects of social media use on mental health and wellbeing among young people in England: A secondary analysis of longitudinal data. The Lancet Child & Adolescent Health, 3(10), 685–696. https://doi.org/10.1016/S2352-4642(19)30186-5
Wade, N. E., Ortigara, J. M., Sullivan, R. M., Tomko, R. L., Breslin, F. J., Baker, F. C., Fuemmeler, B. F., Delrahim Howlett, K., Lisdahl, K. M., Marshall, A. T., Mason, M. J., Neale, M. C., Squeglia, L. M., Wolff-Hughes, D. L., Tapert, S. F., & Bagot, K. S. (2021). Passive sensing of preteens’ smartphone use: An adolescent brain cognitive development (ABCD) cohort substudy. JMIR Mental Health, 8(10), Article e29426. https://doi.org/10.2196/29426
Wang, Z., Emmerich, A., Pillon, N. J., Moore, T., Hemerich, D., Cornelis, M. C., Mazzaferro, E., Broos, S., Ahluwalia, T. S., Bartz, T. M., Bentley, A. R., Bielak, L. F., Chong, M., Chu, A. Y., Berry, D., Dorajoo, R., Dueker, N. D., Kasbohm, E., Feenstra, B., … Hoed, M. den. (2022). Genome-wide association analyses of physical activity and sedentary behavior provide insights into underlying mechanisms and roles in disease prevention. Nature Genetics, 54(9), 1332–1344. https://doi.org/10.1038/s41588-022-01165-1
Wen, H., Sobolev, M., Vitale, R., Kizer, J., Pollak, J. P., Muench, F., & Estrin, D. (2021). mPulse mobile sensing model for passive detection of impulsive behavior: Exploratory prediction study. JMIR Mental Health, 8(1), Article e25019. https://doi.org/10.2196/25019
Wendt, F. R., Muniz Carvalho, C., Pathak, G. A., Gelernter, J., & Polimanti, R. (2019). Deciphering the biological mechanisms underlying the genome-wide associations between computerized device use and psychiatric disorders. Journal of Clinical Medicine, 8(12), Article 2040. https://doi.org/10.3390/jcm8122040
Yang, Z., Asbury, K., & Griffiths, M. D. (2019). “A cancer in the minds of youth?” A qualitative study of problematic smartphone use among undergraduate students. International Journal of Mental Health and Addiction, 19(4), 934–946. https://doi.org/10.1007/s11469-019-00204-z
Zhao, S., Xu, F., Xu, Y., Ma, X., Luo, Z., Li, S., Dey, A., & Pan, G. (2019). Investigating smartphone user differences in their application usage behaviors: An empirical study. CCF Transactions on Pervasive Computing and Interaction, 1(2), 140–161. https://doi.org/10.1007/s42486-019-00011-4
Authors' Contribution
Silvia Marin-Dragu: conceptualization, methodology, statistical analysis, writing—original draft, writing—review & editing. Matt Orr: writing—review & editing. Benjamin Rusak: writing—review & editing. Penny Corkum: conceptualization, statistical analysis, writing—review & editing. Alexa Bagnell: writing—review & editing. Sandra Meier: conceptualization, methodology, statistical analysis, writing—review & editing, project administration, supervision.
Editorial Record
First submission received:
October 21, 2023
Revisions received:
July 11, 2024
November 27, 2024
May 20, 2025
August 13, 2025
Accepted for publication:
October 20, 2025
Editor in charge:
David Smahel
Introduction
Excessive screen-time has been consistently found associated with depression, anxiety, conduct disorders, and attention problems in young people (Eirich et al., 2022; Elhai et al., 2020; Li et al., 2021; Yang et al., 2019). The COVID-19 pandemic and subsequent public-health-mandated restrictions have further fostered a strong reliance on digital media for nearly all facets of daily life (e.g., schooling, socialization, entertainment), thereby resulting in dramatic increases in screen-time among youths. Specifically, a recent meta-analysis including 46 studies suggested that screen-time increased by over 50% during the pandemic (Madigan et al., 2022). Thus, excessive screen-time can be considered a major public health concern for young people and understanding the association of screen-time with mental health problems may help inform the development of policies and interventions to promote healthy screen use and better mental health in young people.
While research has consistently linked screen-time with poor mental health, the direction of the association remains unclear. While it is plausible that excessive screen-time could contribute to mental health issues, existing mental health challenges could also drive increased screen use; for example, young people experiencing anxiety or depression may turn to screens for distraction or social connection, potentially reinforcing a negative cycle (Twenge & Campbell, 2018).
Numerous mechanisms could account for the association between screen-time and mental health problems. Some recent studies have highlighted that prolonged screen-time, particularly on mobile devices, is linked to fragmented attention and reduced cognitive control, heightening stress and contributing to anxiety and depression (Santos et al., 2024). Social isolation, disrupted sleep, reduced physical activity and exposure to nature have also been found as additional mechanisms (Deyo et al., 2024; Twenge & Campbell, 2018; Verma et al., 2022). Overall, it appears that displacement hypothesis offers a key explanation. Displacement hypothesis posits that screen-time indirectly affects mental health because it displaces time participating in healthier activities, such as sleep, physical activity, and social exchanges known to foster mental health (Cain & Gradisar, 2010; Exelmans & Van den Bulck, 2019). Among these factors, the indirect pathway through sleep warrants particular attention, as over 72% of youths report checking their screens as the last activity before falling asleep (Government of Canada, 2021a). Importantly, research consistently demonstrated a strong association between screen-time and poor sleep quality (Hale & Guan, 2015), which, in turn, is a significant predictor of mental health issues (Alonzo et al., 2021; Cavalli et al., 2021; Guerrero et al., 2019; Leung & Torres, 2021; Li et al., 2019). The mechanisms hypothesized to underlie this relationship include disruptions caused by social media notifications (Godsell & White, 2019), suppression of melatonin and subsequent circadian rhythm disturbances due to screen exposure (Touitou et al., 2016), and increased stress or worry from cyberbullying and technology-driven social comparison (Hoge et al., 2017; Landoll et al., 2015; Viner et al., 2019). Yet, screen-time may also have direct effects on mental health independent of sleep. For example, Elhai et al., (2019) found that excessive screen-time, particularly on social media, directly correlates with symptoms of depression and anxiety. Additionally, studies have highlighted poor self-regulation and emotional coping in youth who spend prolonged time on screen (Landoll et al., 2015; Vernon et al., 2018). Thus, both direct and indirect effects warrant investigation.
Despite the growing body of evidence, findings remain mixed, with some studies failing to identify significant associations between screen-time and mental health (Przybylski & Weinstein, 2017). Methodological differences, such as subjective self-report measures, variability in screen-time definition, and differences in population demographics, may account for these inconsistencies. Researchers underscore that longitudinal studies and the use of objective measurement tools remain crucial for disentangling and better understanding the directionality of these associations (Orben & Przybylski, 2019). Most studies on screen-time and mental health rely on subjective self-reports, which are often inaccurate due to underreporting (Arundell et al., 2019; Da Costa et al., 2021; Wade et al., 2021). Self-reported data is frequently biased by recall errors, social desirability, and inconsistent interpretation of screen-time activities (Boase & Ling, 2013; Parry et al., 2021). Such tools leverage smartphone sensors to unobtrusively and accurately track screen-time, offering a more reliable assessment of actual device usage (Dissing et al., 2022; Druijff-van de Woestijne et al., 2021; Meyerhoff et al., 2021; Torous et al., 2016). Objective measures have also been shown to capture nuanced usage patterns, such as nighttime usage, which are often missed in self-report surveys (Ellis et al., 2019). As a result, novel, objective measurement methods are needed (Borger et al., 2019; Wade et al., 2021). Moreover, considering that different operating systems emphasize distinct designs around aspects such as parental controls (Peltonen et al., 2018), the type of operating system may impact potential associations. Importantly, mobile sensing apps implemented on most devices have already been shown to successfully measure screen-time in youths (MacLeod et al., 2021; Wade et al., 2021).
Additionally, demographic factors such as sex and maternal education may influence the relationship between screen-time, sleep, and mental health. Research indicates sex-based differences in smartphone usage, sleep behaviours, and the prevalence of externalizing and internalizing symptoms (Atherton et al., 2018; Godsell & White, 2019). Furthermore, maternal education has been linked to youth mental health outcomes (Hosokawa & Katsura, 2017), suggesting that these variables are critical for understanding the broader impact of screen-time.
Thus, the primary objective of the present study was to determine whether smartphone screen-time objectively measured via a mobile sensing app is associated with poorer mental health in young people. The secondary objective was to examine whether screen-time is directly associated with poorer mental health or indirectly through its impact on sleep. Specifically, we assessed whether sleep duration mediates the relationship between screen-time and mental health outcomes.
We hypothesized that:
H1: High levels of objectively measured smartphone screen-time would be associated with poorer mental health.
H2: Screen-time would lead to reduced sleep, which, in turn, would negatively affect mental health.
Methods
Sample
The sample consisted of 550 young people, aged 15–25 years, who spoke fluent English and owned a smartphone (iOS or Android). The data were collected between June 2020 and November 2021. Participants in inpatient mental health treatment were excluded from the study. Participants were recruited through online methods, such as university electronic platforms (SONA), social media platforms (e.g., Instagram, Facebook) and Canadian ad sites (Kijiji). Table 1 and 2 detail the characteristics of the sample and variables included in the analysis. It consisted of 407 participants, with an average age of 20.94 years (SD = 2.5). Biological sex was reported as female by 84% of the sample (342 participants). In terms of phone operating system, 74% of participants (302) used an iOS device, and 26% (105) used the Android operating system. For ethnical background, participants could select one or more categories, depending on their identity; as such, 24% participants identified as Asian, 3% as Black/African, 68% as White, 3% identified as Hispanic, 3% as Indigenous, less than one percent as Pacific Islander, and 9% opted for Other or preferred not to answer the question. Maternal education was used as a substitute for socioeconomic status, and 5% of participants reported that their mother’s did not finish high school education, 17% reported that their mother’s education included graduating from high-school, 22% reported further education beyond high-school, while 54% reported university level education, with the rest of the participants reporting that they did not know or preferred not to answer this question.
Procedure and Consent
Potential participants were guided through detailed information regarding study procedures and consent via “REDCap,” a platform specifically designed to conduct online studies (Garcia & Abrahão, 2021) and approved by provincial health authorities. First, REDCap offered detailed information about the purpose and steps of the study and provided opportunities to request more information or ask questions. Then participants provided their consent to participate in the study through their online signature via REDCap. Next, participants provided demographic information and completed the questionnaire (SDQ). After completing this step, participants were provided with detailed instructions on installing and downloading the mobile sensing app (PROSIT) and were recommended to use it for at least 14 consecutive days; some participants opted to use the app for a longer period. All study procedures were consistent with the Declaration of Helsinki and were approved by the Dalhousie University Research Ethics Board. Participants received a $60 CAD (approx. 37 EUR) gift card as compensation for their time.
Measures
Objective Duration of Smartphone Screen-Time
Duration of average daily screen-time, in seconds, was assessed through the PROSIT app (previously described in detail elsewhere (MacLeod et al., 2021). The app runs automatically in the background, and it does not need user input to monitor smartphone use behaviour. All collected data were uploaded to secure databases at Dalhousie University. After quality control preprocessing (excluding participants with screen-time longer than 10 hours per day, likely due to device misuse or technical errors, as well as participants who had less than 14 days of app data collected), the duration of smartphone screen-time was calculated by summing the intervals between the time when the user turned on the device and actively used it and when the screen was turned off. This passive, low-burden method of data collection has been suggested to provide a more accurate measure of daily screen-time than subjective self-reports (Parker et al., 2022; Wade et al., 2021).
Sleep Duration
Duration of average daily sleep, in seconds, was similarly assessed through the PROSIT app. In line with previous work, a validated sleep algorithm was employed to identify the nighttime intervals when the device was not in use, which would suggest a sleep episode (Ciman & Wac, 2019). To ensure high data quality, sleep intervals were required to last longer than 4 hours and less than 10 hours and had to occur between 9 p.m. and 9 a.m. While actigraphy is widely used to objectively measure sleep (Ancoli-Israel et al., 2003), in the context of this study the outlined method of determining sleep based on screen interactions seemed preferable as actigraphy was observed to misclassify bedtime screen use as a period of sleep (Borger et al., 2019; Otte Andersen et al., 2022).
Youth Mental Health
The Strengths and Difficulties Questionnaire (SDQ; Goodman, 1997) was used as a measure of youth mental health due to its high concurrent validity with other means of assessing youth mental health (Goodman & Scott, 1999), its fair internal consistency (α =.73), and test-retest reliability (.62; Goodman, 2001).The questionnaire asks the participant to rate 25 affirmations on a three-point Likert scale and provides an assessment of two main factors – internalizing (e.g., anxiety, depression) and externalizing (e.g., impulsivity, aggression) symptoms. Higher scores are indicative of greater numbers of symptoms. In our sample, the findings aligned with previous results, obtaining a Cronbach’s Alpha of .75 for the internalizing subscale, and an Alpha value of .68 for the externalizing subscale.
Covariates
Demographic data were collected using an adapted Statistics Canada self-report questionnaire (Government of Canada, 2021b), including age, biological sex, current mental health treatment, maternal education and type of smartphone operating system used. We controlled for the current mental health treatment based on participants’ self-reports to account for any potential biases. In addition, maternal education was used as a substitute for socioeconomic status, being considered a good proxy for this type of information (Jackson et al., 2017). Finally, phone operating system type (Android or iOS) was examined as a potential covariate in a sensitivity analysis, due to the fact that previous studies have highlighted that users of different operating systems (e.g., iOS and Android) may have varying usage patterns due to difference in app ecosystems, user interfaces and demographic factors (Benenson et al., 2013; Zhao et al., 2019).
Data Analysis
Analyses were conducted in the period of January–March 2022. There were 550 participants invited to the study, and 20 individuals declined to participate. We excluded 79 participants with values of screen-time that were considered extreme (screen-time over 10 hours per day, which is 3 or more times the usually observed screen-time (Li et al., 2021; Nagata et al., 2021), who had inconsistent technical data, or who had less than 14 days of app data collected. Forty-four participants who did not have qualifying sleep data were also excluded. Among the remaining 407, some participants opted not to answer one or more items on the mental health questionnaire (SDQ), which precluded the calculation of a total score on the internalizing or externalizing symptom scores. We excluded 26 participants with these missing values on internalizing and 18 on externalizing symptoms from further analysis. We compared this subsample (n = 407) to the full sample who started the study (n = 530) using independent samples t-tests and χ²-tests. There were no statistically significant differences observed between groups in terms of age, biological sex, maternal education, current treatment status, internalizing or externalizing symptoms (all p >.05). We thus continued our analysis with the subsample (n = 407). We first calculated descriptive statistics (presented below in Tables 1 and 2). Our results showed that participants used the app for an average of 31.41 days (SD = 11.01) during the study, and the mean duration of objectively measured smartphone screen-time per day was approximately 3.57 hours (SD = 1.71). The average duration of sleep per day recorded by the app was 7.44 hours (SD = 0.99).
Table 1. Sociodemographic Characteristics of Participants.
|
Characteristic |
n (%) |
Total |
|
Biological Sex |
|
407 |
|
Female |
342 (84) |
|
|
Male |
65 (16) |
|
|
Phone Type |
|
407 |
|
Android |
105 (26) |
|
|
iOS |
302 (74) |
|
|
Current Mental Health Treatment |
|
407 |
|
Yes |
85 (19) |
|
|
No |
322 (71) |
|
|
Mother’s education |
|
407 |
|
Did not finish High school |
19 (5) |
|
|
Finished High school |
70 (17) |
|
|
Further education |
91 (22) |
|
|
University |
221 (54) |
|
|
I don’t know |
3 (<1) |
|
|
Prefer not to answer |
3 (<1) |
|
|
Ethnical background |
|
407 |
|
Asian |
99 (24) |
|
|
Black/African |
13 (3) |
|
|
White |
278 (68) |
|
|
Hispanic |
11 (3) |
|
|
Indigenous |
12 (3) |
|
|
Pacific Islander |
1 (<1) |
|
|
Other |
36 (9) |
|
Table 2. Descriptive Statistics (Mean, Standard Deviation).
|
Variable |
M |
SD |
|
Age |
20.94 |
2.5 |
|
PROSIT app use |
31.41 |
11.01 |
|
Screen-time |
3.57 |
1.71 |
|
Sleep per day |
7.44 |
0.99 |
Next to test our hypotheses, a single structural equation model (SEM) was specified using the “lavaan” package (Rosseel, 2012). Specifically, the model evaluated whether objectively measured smartphone screen-time was associated with internalizing and externalizing symptoms, and whether these associations were mediated by sleep duration. Internalizing and externalizing symptoms were specified as second-order latent variables, defined by subscale-level first-order latent constructs from the Strengths and Difficulties Questionnaire (SDQ). Internalizing symptoms were represented by their corresponding latent constructs/subscales (i.e., peer problems and emotional symptoms), while externalizing symptoms were represented by their corresponding subscales (i.e., conduct and hyperactivity symptoms). The predictors included screen-time, current mental health treatment, biological sex and maternal education. Covariance between the outcomes was also estimated to account for the expected correlation between these symptom dimensions. The model was estimated using Diagonally Weighted Least Squares Mean and Variance adjusted estimation to handle missing data and ensure unbiased parameter estimates. Bootstrapped standard errors and confidence intervals were computed using 1,000 resamples. The analysis included 379 observations out of the original 407, with missing data handled by the pairwise deletion mechanism intrinsic to the WLSMV estimator. The missingness in the data was evaluated using Little’s MCAR test to assess whether the data were missing completely at random. Little's MCAR test identified three distinct missingness patterns across the main variables; the majority of cases (379) had complete data, while two smaller groups exhibited partial missingness. The Hawkins test for normality and homoscedasticity yielded a p-value of .281, indicating that there is no significant evidence against the assumption that the missing data are MCAR.
In addition, we conducted the following sensitivity analyses. First, because different operating systems (e.g., iOS and Android) can affect screen-time measures (Benenson et al., 2013; Zhao et al., 2019), we assessed differences in screen-time by operating system using an independent samples t-test. Results revealed a significant difference between groups; t(174.62) = 3.96, p < .001. Accordingly, we adjusted the SEM models outlined above for operating systems, presenting results in Tables 5 and 6. Second, as the association between screen-time and youth mental health may differ across mental health profiles (Fassi et al., 2025), we conducted multi-group path analyses comparing youth currently receiving mental health treatment to those not in treatment. Following recommendations by van de Schoot et al. (2012), we tested a series of increasingly restrictive models to evaluate group invariance. Model 1 assessed configural invariance by fitting the same model in both groups without equality constraints. Model 2 tested intercept invariance by constraining the intercepts to be equal across groups. Model 3 further constrained the regression coefficients to be equal between groups. Model comparisons were evaluated using nested model fit indices, including Δχ² tests with non-significant p-values, ΔCFI < 0.01, and ΔRMSEA < 0.015, as recommended by Chen (2007) and Cheung & Rensvold (2002). R statistical software version 4.1.2 (R Project for Statistical Computing) was used for all analyses (Giorgi et al., 2022).
Results
An SEM model was estimated to examine whether objectively measured smartphone screen-time was associated with internalizing and externalizing symptoms in youth, and whether these associations were mediated by sleep duration. The model demonstrated adequate fit to the data, χ²(255) = 447.56, p < .001, CFI = .937, TLI = .928, RMSEA = .041; 90% CI [.033, .048], and SRMR = .061. The main model’s results are presented below in Table 3 and Figure 1, and the covariates’ effects are presented in Table 4.
Figure 1. Sleep as a Mediator of the Relationship Between Duration of Smartphone-Based
Screen-time and Externalizing Symptoms, Using Standard Coefficients.
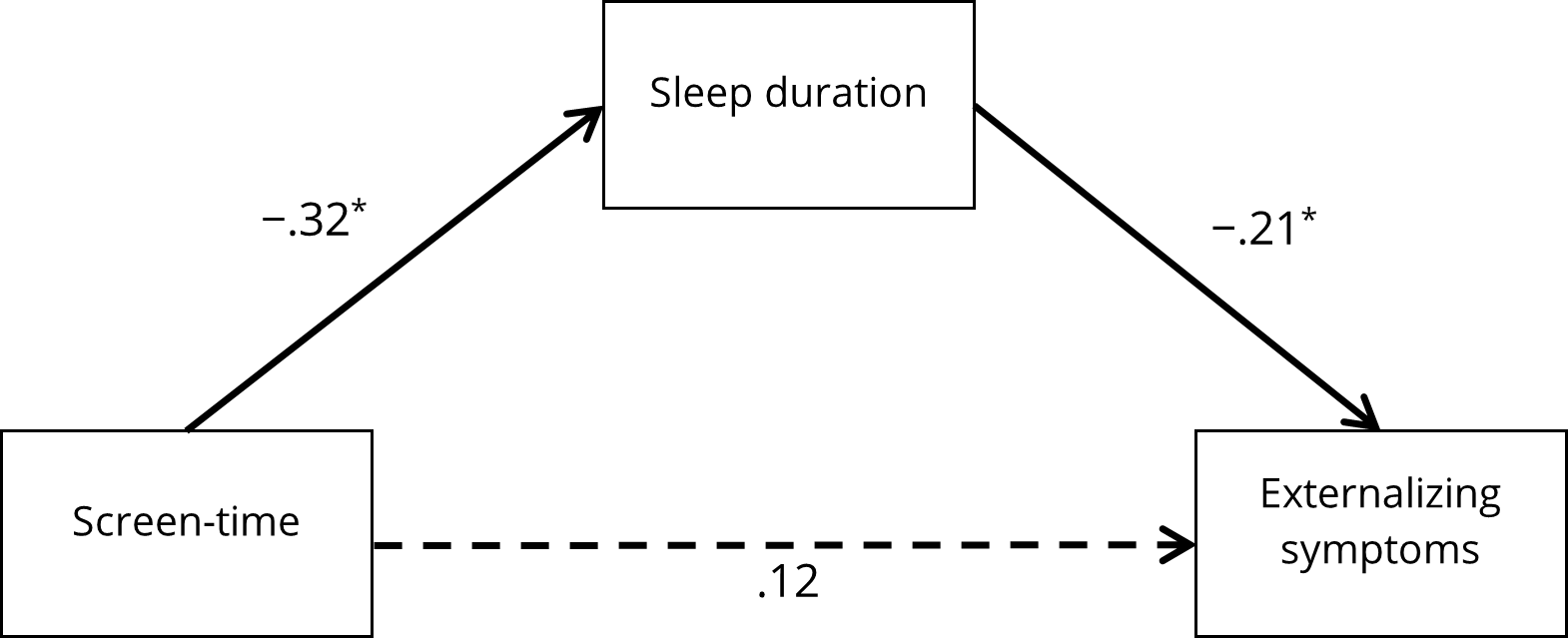
Note. Standardized parameter estimates are reported. Dotted lines indicated non-significant parameters.
Covariates were not depicted for the sake of simplicity. Full arrows indicate significant paths. * p < .05.
Screen-time was not directly associated with externalizing symptoms; β = .118, SE = .023, p = .212, 95% CI [–.011, .078]. However, there was a significant indirect effect via sleep duration; β = .067, SE = .007, p = .016, 95% CI [.016, .089], indicating that higher screen-time was related to shorter sleep, which in turn was associated with greater externalizing symptoms. The total effect of screen-time on externalizing symptoms was also significant; β = .185, SE = .022, p = .042, 95% CI [.003, .085].
In contrast, screen-time was not significantly associated with internalizing symptoms either directly; β = .094, SE = .013, p = .178, 95% CI [–.005, .048] or indirectly through sleep; β = .032, SE = .004, p = .155, 95% CI [–.003, .047]. The total effect of screen-time on internalizing symptoms was also nonsignificant; β = .126, SE = .013, p = .073, 95% CI [–.007, .049].
Among the covariates, not being in current mental health treatment was significantly associated with shorter sleep duration (β = –.102, p = .030), higher externalizing symptoms (β = .278, p < .001), and higher internalizing symptoms (β = .267, p = .001), relative to those currently in treatment. Biological sex was significantly associated with greater sleep duration (β = .142, p = .003) and more internalizing symptoms (β = .209, p = .003) among males, but no differences were observed in externalizing symptoms. Higher maternal education was significantly related to fewer externalizing symptoms (β = –.169, p = .018) but was not significantly associated with sleep duration or internalizing symptoms.
Table 3. Structural Equation Results Depicting Effects of Screen-Time on Externalizing and Internalizing Symptoms via Sleep Duration.
|
Outcome |
B |
SE |
95% CI [LL, UL] |
p-value |
β |
|
Externalizing |
|
|
|
|
|
|
Direct effect (screen-time → externalizing) |
.028 |
.023 |
[−.011, .078] |
.212 |
.118 |
|
Indirect effect (screen-time → sleep → externalizing) |
.016 |
.007 |
[.016, .089] |
.016 |
.067 |
|
Total effect (screen-time → externalizing) |
.044 |
.022 |
[.003, .085] |
.042 |
.185 |
|
Internalizing |
|
|
|
|
|
|
Direct effect (screen-time → internalizing) |
.018 |
.013 |
[−.005, .048] |
.178 |
.094 |
|
Indirect effect (screen-time → sleep → internalizing) |
.006 |
.004 |
[−.003, .047] |
.155 |
.032 |
|
Total effect (screen-time → internalizing) |
.024 |
.013 |
[−.007, .049] |
.073 |
.126 |
|
Note. B = unstandardized estimate; SE = standard error; CI = confidence interval; β = standardized estimate. Results are adjusted for current mental health treatment, biological sex and maternal education. |
|||||
Table 4. Covariate Effects on Sleep Duration and Internalizing and Externalizing Symptoms.
|
Outcome |
Covariate |
B |
SE |
95% CI [LL, UL] |
p-value |
β |
|
Sleep Duration |
|
|
|
|
|
|
|
|
Current Treatment |
−.252 |
.116 |
[−.482, −.025] |
.030 |
−.102 |
|
|
Biological Sex |
.386 |
.130 |
[.130, .633] |
.003 |
.142 |
|
|
Mother’s Education |
.046 |
.051 |
[−.054, .147] |
.359 |
.046 |
|
Externalizing |
|
|
|
|
|
|
|
|
Current Treatment |
.162 |
.043 |
[.071, .242] |
<.001 |
.278 |
|
|
Biological Sex |
.014 |
.046 |
[−.064, .121] |
.767 |
.021 |
|
|
Mother’s Education |
−.04 |
.017 |
[−.074, −.008] |
.018 |
−.169 |
|
Internalizing |
|
|
|
|
|
|
|
|
Current Treatment |
.125 |
.038 |
[.060, .214] |
.001 |
.267 |
|
|
Biological Sex |
.107 |
.036 |
[.043, .182] |
.003 |
.209 |
|
|
Mother’s Education |
−.001 |
.011 |
[−.024, .021] |
.948 |
−.004 |
|
Note. B = unstandardized estimate; SE = standard error; CI = confidence interval; β = standardized estimate. Please note that current mental health treatment has been coded as 1 when not in treatment and 0 as in treatment; for biological sex, female participants are coded as 0 and male participants as 1. |
||||||
Sensitivity Analyses
In sensitivity analyses, we first added smartphone operating system as a covariate to the main model. The model fit was adequate, χ²(273) = 469.12, p < .001, CFI = .937, TLI = .928, RMSEA = .044; 90% CI [.037, .050], SRMR = .060. The results indicated that the indirect effect of screen-time on externalizing symptoms via sleep remained significant (β = .062, p = .020). Moreover, the direct effect of screen-time on externalizing symptoms remained non-significant (β = .124, p = .184), and the total effect was significant (β = .186, p = .040). For internalizing symptoms, no significant direct (β = .088, p = .200), indirect (β = .016, p = .433), or total effects (β = .104, p = .137) were observed. The results also indicated that the covariate smartphone operating system had a significant effect on sleep duration, such that iOS users reported longer sleep than Android users (β = .325, p < .001). Phone operating system was not significantly associated with externalizing symptoms (β = .080, p = .343) or internalizing symptoms (β = –.121, p = .102). Detailed results are presented in Table A1 and Table A2 (Appendix).
Next, we conducted multi-group comparisons by current mental health treatment status by comparing three nested models. Configural invariance (Model 1), invariance of the intercepts (Model 2), and invariance of the regression coefficients (Model 3) were tested. The model comparison showed that the values across Model 1 and Model 2 (Δχ2 = 22.583, df = 15, p = .093) and Models 1 and Model 3 (Δχ2 = 42.714, df = 33, p = .120) didn’t differ. Adding the equality constraints on the intercepts and regression coefficients didn’t worsen model fit; this indicated that youth currently receiving mental health treatment don’t need to be separately analyzed from those not in treatment. Therefore, a model across both mental health profiles was fitted, which demonstrated adequate fit to the data, χ²(237) = 420.35, p < .001, CFI = .939, TLI = .929, RMSEA = .049, 90% CI [.041, .056], and SRMR = .061. The model’s results are presented below in Table A3 and Figure A1 (Appendix).
Screen-time was not directly associated with externalizing symptoms; β = .123, SE = .023, p = .183, 95% CI [–.012, .079]. However, there was a significant indirect effect via sleep duration; β = .079, SE = .008, p = .011, 95% CI [.006, .036], indicating that higher screen-time was related to shorter sleep, which in turn was associated with greater externalizing symptoms. The total effect of screen-time on externalizing symptoms was also significant; β = .202, SE = .022, p = .023, 95% CI [.009, .095].
In contrast, screen-time was not significantly associated with internalizing symptoms either directly; β = .098, SE = .015, p = .207, 95% CI [–.006, .053] or indirectly through sleep; β = .044, SE = .005, p = .091, 95% CI [−.000, .095]. The total effect of screen-time on internalizing symptoms was also nonsignificant; β = .142, SE = .016, p = .075, 95% CI [–.002, .064].
Discussion
The study aimed to investigate the relationship between smartphone screen-time, sleep duration, and mental health outcomes. Two main hypotheses were tested: 1) whether high levels of objectively measures smartphone screen-time were associated with poorer mental health and 2) whether screen-time contributed to reduced sleep duration, which in turn would negatively affect mental health, supporting displacement hypothesis that suggests screen-time may disrupt sleep and subsequently impact mental well-being.
In the present study, the hypotheses were partially supported. Using objective measures, our results highlighted that screen-time was not directly associated with internalizing or externalizing symptoms; however, there was a significant indirect association between screen-time and externalizing symptoms, pointing to a relationship mediated by other factors, in this case, sleep duration. In contrast, no significant associations were found between screen-time and internalizing symptoms, and sleep did not significantly mediate this relationship.
Sensitivity analyses confirmed that results remained robust after additional adjustments for the operating system. Similarly, multi-group comparisons indicated that the estimated paths and effects were consistent for both youths currently receiving mental health treatment and those who were not.
Our findings align with some longitudinal (Johnson et al., 2007; Ra et al., 2018) and cross-sectional (Mathers et al., 2009) studies that found a significant link between screen-time and poor mental well-being in youth. In contrast, other studies suggest the directionality of the association is not as clear as children enter preadolescence and that other factors (such as problematic behaviours, family environment) could impact the association between sleep, screen-time, and mental health (Boers et al., 2019; H. Cao et al., 2011; Ferguson, 2011; Primack et al., 2009; Riehm et al., 2019; Sanders et al., 2019).
A meta-analysis including over 87 studies employing subjective measures of screen-time indicated that while high levels of screen-time were associated with higher levels of internalizing and externalizing symptoms, the association with screen-time was significantly stronger for externalizing symptoms (Eirich et al., 2022). Genetic studies similarly provided evidence for higher correlations of genetic underpinnings of screen-time with externalizing than internalizing symptoms (Wang et al., 2022; Wendt et al., 2019). Our results are therefore consistent with a stronger linkage of higher screen-time with externalizing symptoms.
The study’s findings are based on objectively obtained data, and as previously outlined, studies using mobile sensing technology to determine the association of screen-time with mental health problems are scarce. Pilot studies using mobile sensing apps to measure screen-time provided inconsistent findings for and against an association of screen-time with internalizing symptoms (J. Cao et al., 2020; MacLeod et al., 2021). Similarly, a small pilot study (Wen et al., 2021) involving 26 participants found multiple correlations between objectively measured screen-time with externalization/impulsivity traits (such as non-planning, perseverance and sensation seeking).
Some literature suggests that the association of screen-time with externalizing symptoms represents a direct causal effect. Specifically, the fast-paced and intense audiovisual effects of digital media may encourage attention to quickly shift, increase arousal and impede self-regulation strategies, which may be associated with externalizing symptoms (Eirich et al., 2022; Madigan et al., 2019). In our study, the effect of screen-time on externalizing symptoms was primarily mediated by reduced sleep, supporting the hypothesis of indirect causality, consistent with a displacement interpretation; namely, that the effects of additional screen time are mediated by displacing sleep. Compatible with our findings, a recent study that used subjective measures similarly observed that screen-time exacerbates externalizing symptoms indirectly through increased sleep disturbances (Cavalli et al., 2021). For internalizing symptoms, studies provided inconsistent results concerning the mediating role of sleep (Leung & Torres, 2021; Li et al., 2019).
Adequate sleep is vital for adolescent brain function and behaviour because of its involvement in brain development, learning, memory, and emotion regulation (Tarokh et al., 2016). Thus, a reduction in sleep can be expected to contribute to the development of mental health problems. Considering potential pathological mechanisms, screen-time may interfere with sleep by substituting for sleep time, delaying sleep onset, or causing disruptions from nighttime notifications and fear of missing out (Godsell & White, 2019; Tandon et al., 2021). Furthermore, technology-based stressors like cyberbullying and social comparisons may contribute to sleep difficulties (Hoge et al., 2017; Landoll et al., 2015; Viner et al., 2019). Light exposure from screens can also supress melatonin production and disrupt physiological processes linked to sleep (Chang et al., 2015; Combertaldi et al., 2021; Heo et al., 2017) and may even contribute to neuroinflammation (Verma et al., 2022).
Although the effect sizes found in this study are small, the consequences of excessive screen-time at a population level are likely meaningful, as so many youth exceed screen-time guidelines (Tapia-Serrano et al., 2022). Therefore, interventions are urgently needed to promote healthy screen use in youth. There is evidence that interventions that promote media literacy can change attitudes and intentions to engage in screen use (Vahedi et al., 2018). In addition, a recent randomized clinical trial showed that interventions reducing screen-time can boost engagement in more health-promoting activities (Pedersen et al., 2022).
Strengths and Limitations
To the best of our knowledge, our study is one of the first to investigate the potential effect of sleep as a mediator of the association between smartphone screen-time and youth mental health using objective measures. This objectivity is a major strength as it addresses the challenges posed by more subjective measures, such as self-report, in studying the effects of screen-time (Neville et al., 2021).
However, the study also has multiple limitations. Because of its design, this study could only evaluate associations between variables; the causality and directionality of these associations cannot be inferred. Results are further limited by the inability of passive mobile sensing techniques to capture all screen use (such as television, and computer). Future research should consider collecting more granular and in-depth data regarding cross-media usage patterns. However, given the dramatic increases in young people’s use of digital media in recent years, there is unique value in measuring and investigating this form of screen-time specifically (McDaniel & Radesky, 2020). Measuring sleep objectively, through smartphone interactions, might be viewed as a good still very new alternative to other technologies such as actigraphy (Borger et al., 2019), having the advantage of reaching a larger number of participants and assessing behaviour in a naturalistic manner. This type of assessment becomes more salient for younger participants, since many of them report using their phone in bed, awake, while engaging in very little physical movement (Vernon et al., 2018). However, the limitation that needs to be considered is that the technology is still in the early phases of development, compared to actigraphy, which has been researched and validated over a longer period of time.
In addition, not all screen-time may have a detrimental impact on youth mental health. The pandemic has underscored that young people also use screens for positive purposes, such as education or entertainment (Ribner et al., 2021) and social interactions with peers, family, and other people important to them (Pang, 2022). A recent study (Liu et al., 2023) found that the link between screen-time (e.g., social media, movie viewing) with anxiety and depressive symptoms varied by type of screen viewing. As such, more nuanced aspects of screen-time, such as screen content (e.g., social media, games), context (e.g., active vs. passive use), and motives (e.g., social contact, education, entertainment), should accordingly be examined in future studies.
Furthermore, the algorithm employed to quantify sleep in this study may be considered too simple in its current form and may require further validation. Considering that sleep is a multidimensional concept (Buysse, 2014) and taking advantage of the multitude of other sensors available, richer contextual information could be gathered to generate estimates of other sleep features, such as sleep onset latency, sleep quality, sleep duration during weekdays and weekends, and diurnal variation (Joshi, 2022). To confirm the quality of these estimates, additional objective measures could be used to corroborate the findings, such as through actigraphy or sleep studies. Moreover, other variables that are known to interact with sleep and mental health should be investigated, such as physical activity (H. Cao et al., 2011; Wang et al., 2022). Additionally, future studies that include a larger sample and more in-depth screen-time information may be able to better discern whether specific types of smartphone use have a direct effect on externalizing symptoms and whether they are mediated by sleep duration. In particular, considering the sensitivity analyses results, replication in larger and more balanced samples could help to confirm patterns. Another limitation may be derived from the fact that the majority of the sample was female, and this aspect may impact the generalizability of results. While female participants are more likely to volunteer to participate in research (Galea & Tracy, 2007), we must take into consideration that girls and young women are more likely to experience psychological distress due to mobile device use, particularly through the detrimental effects of social media (Abi-Jaoude et al., 2020). Finally, this study might have limited generalizability since it took place during the COVID-19 pandemic period and it relied on cross-sectional data, which can bias mediation estimates and may not fully represent longitudinal causal relationships (Maxwell et al., 2011).
Conclusions
The association between screen-time and youth mental health has garnered marked attention from the academic, health, and public sectors. In this study making use of the objective methodology of mobile sensing, smartphone screen-time was significantly associated with externalizing symptoms, which was explained by reduced nighttime sleep duration. Our study thereby complements those studies using subjective measures of screen-time in cross-sectional designs or longitudinal cohorts, indicating the need for further investigation of the relationship between screen-time use and youth mental health. Our findings may also help inform interventions to boost media literacy and reduce screen-time in favor of more health-promoting activities.
Conflict of Interest
The authors have no conflicts of interest to declare.
Use of AI Services
The authors declare they have not used any AI services to generate or edit any part of the manuscript or data.
Appendix
Table A1. Structural Equation Results Depicting Effects of Screen-Time on Externalizing and Internalizing Symptoms
via Sleep Duration, With Operating System Added as an Additional Covariate.
|
Outcome |
B |
SE |
95% CI [LL, UL] |
p-value |
β |
|
Externalizing |
|
|
|
|
|
|
Direct effect (screen-time → externalizing) |
.030 |
.022 |
[−.012, .077] |
.184 |
.124 |
|
Indirect effect (screen-time → sleep → externalizing) |
.015 |
.006 |
[.003, .028] |
.020 |
.062 |
|
Total effect (screen-time → externalizing) |
.045 |
.022 |
[.006, .091] |
.040 |
.186 |
|
Internalizing |
|
|
|
|
|
|
Direct effect (screen-time → internalizing) |
.017 |
.013 |
[−.005, .048] |
.200 |
.088 |
|
Indirect effect (screen-time → sleep → internalizing) |
.003 |
.004 |
[−.003, .012] |
.433 |
.016 |
|
Total effect (screen-time → internalizing) |
.020 |
.013 |
[−.002, .053] |
.137 |
.104 |
|
Note. B = unstandardized estimate; SE = standard error; CI = confidence interval; β = standardized estimate. Results are adjusted for current mental health treatment, biological sex, maternal education, and operating system. |
|||||
Table A2. Covariate Effects on Sleep Duration and Internalizing and Externalizing Symptoms (Sensitivity Analysis).
|
Outcome |
Covariate |
B |
SE |
95% CI [LL, UL] |
p-value |
β |
|
Sleep Duration |
|
|
|
|
|
|
|
|
Current Treatment |
−.214 |
.111 |
[−.433, .004] |
.053 |
−.087 |
|
|
Biological Sex |
.258 |
.129 |
[−.001, .501] |
.045 |
.095 |
|
|
Mother’s Education |
.037 |
.049 |
[−.061, .122] |
.450 |
.037 |
|
|
Phone Type |
.741 |
.117 |
[.506, .980] |
<.001 |
.325 |
|
Externalizing |
|
|
|
|
|
|
|
|
Current Treatment |
.163 |
.045 |
[.072, .256] |
<.001 |
.279 |
|
|
Biological Sex |
.009 |
.047 |
[−.071, .117] |
.851 |
.014 |
|
|
Mother’s Education |
−.040 |
.018 |
[−.075, −.007] |
.022 |
−.170 |
|
|
Phone Type |
.043 |
.046 |
[−.042, .144] |
.343 |
.080 |
|
Internalizing |
|
|
|
|
|
|
|
|
Current Treatment |
.127 |
.038 |
[.060, .212] |
.001 |
.268 |
|
|
Biological Sex |
.115 |
.039 |
[.049, .201] |
.003 |
.221 |
|
|
Mother’s Education |
.001 |
.012 |
[−.026, .022] |
.970 |
−.002 |
|
|
Phone Type |
−.053 |
.032 |
[−.125, .005] |
.102 |
−.121 |
|
Note. B = unstandardized estimate; SE = standard error; CI = confidence interval; β = standardized estimate. Please note that current mental health treatment has been coded as 1 when not in treatment and 0 as in treatment; for biological sex, female participants are coded as 0 and male participants as 1, while phone type was coded as 0 for Android and 1 for iOS. |
||||||
Table A3. Structural Equation Results Across Mental Health Profiles.
|
Outcome |
B |
SE |
95% CI [LL, UL] |
p-value |
β |
|
Externalizing |
|
|
|
|
|
|
Direct effect (screen-time → externalizing) |
.030 |
.023 |
[−.012, .079] |
.183 |
.123 |
|
Indirect effect (screen-time → sleep → externalizing) |
.019 |
.008 |
[.006, .036] |
.011 |
.079 |
|
Total effect (screen-time → externalizing) |
.050 |
.022 |
[.009, .095] |
.023 |
.202 |
|
Internalizing |
|
|
|
|
|
|
Direct effect (screen-time → internalizing) |
.019 |
.015 |
[−.006, .053] |
.207 |
.098 |
|
Indirect effect (screen-time → sleep → internalizing) |
.009 |
.005 |
[−.000, .020] |
.091 |
.044 |
|
Total effect (screen-time → internalizing) |
.028 |
.016 |
[−.002, .064] |
.075 |
.142 |
|
Note. B = unstandardized estimate; SE = standard error; CI = confidence interval; β = standardized estimate. Results are adjusted for biological sex and maternal education. |
|||||
Figure A1. Sleep as a Mediator of the Relationship Between Duration of Smartphone-Based
Screen-Time and Externalizing Symptoms Across Mental Health Profiles.
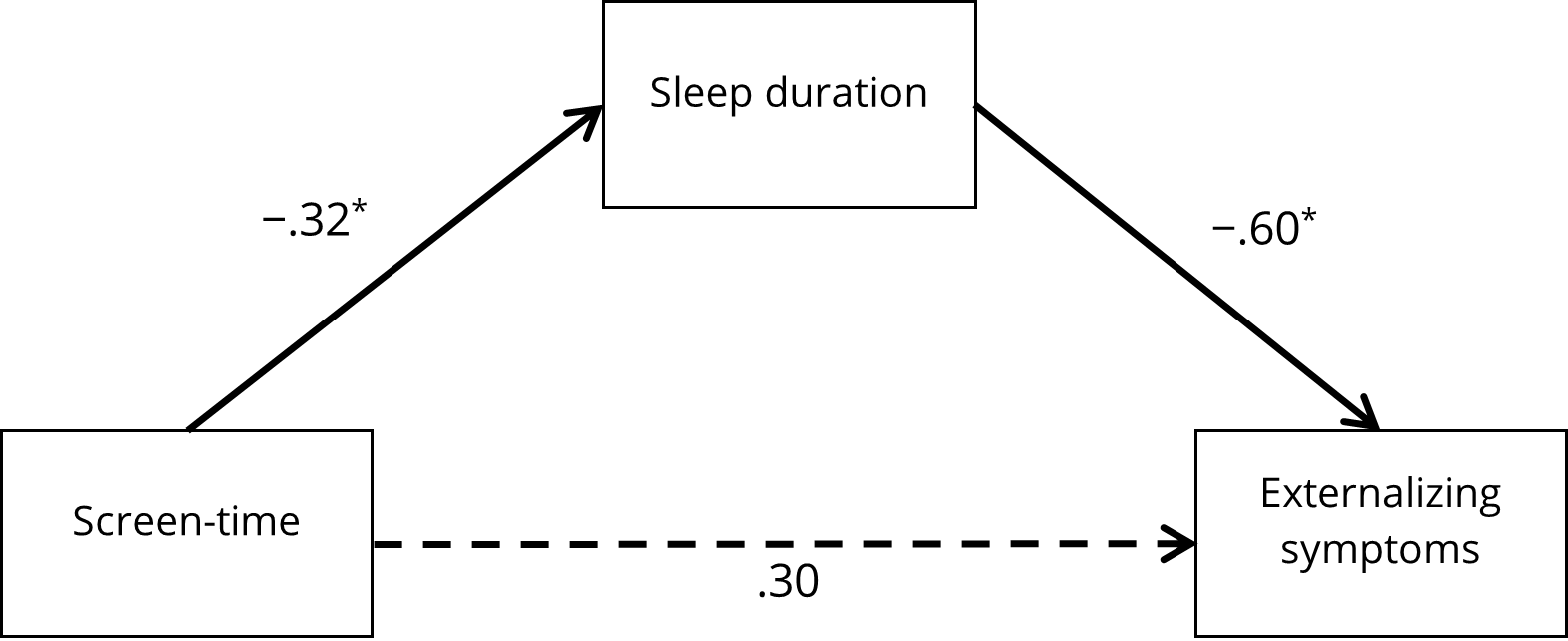
Note. Standardized parameter estimates are reported. Dotted lines indicated non-significant parameters.
Covariates were not depicted for the sake of simplicity. Full arrows indicate significant paths. * p < .05.

This work is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License.
Copyright © 2025 Silvia Marin-Dragu, Matt Orr, Penny Corkum, Benjamin Rusak, Alexa Bagnell, Sandra Meier